COPD awareness Month
What is COPD?
Chronic obstructive pulmonary disease or COPD is a serious lung disease that over time, makes it hard to breathe. You may also have heard COPD called other names, like emphysema or chronic bronchitis. In people who have COPD, the airways—tubes that carry air in and out of your lungs—are partially blocked, which makes it hard to get air in and out.
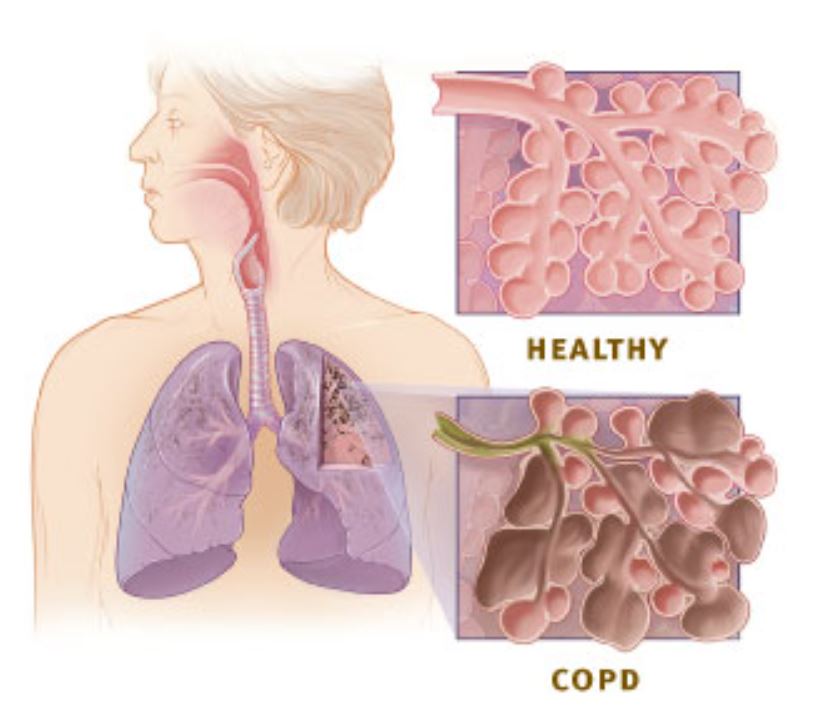
The “airways” are the tubes that carry air in and out of the lungs through the nose and mouth. Healthy airways and air sacs in the lungs are elastic—they try to bounce back to their original shape after being stretched or filled with air, just the way a new rubber band or balloon does. This elastic quality helps retain the normal structure of the lung and helps to move the air quickly in and out.
In people with COPD, the air sacs no longer bounce back to their original shape. The airways can also become swollen or thicker than normal, and mucus production might increase. The floppy airways are blocked, or obstructed, making it even harder to get air out of the lungs.
When COPD is severe, shortness of breath and other symptoms of COPD can get in the way of even the most basic tasks, such as doing light housework, taking a walk, even washing and dressing.
What are the symptoms of COPD?

Symptoms of COPD include:
-
- Frequent coughing or wheezing.
- Excess phlegm, mucus, or sputum production.
- Shortness of breath.
- Trouble taking a deep breath.
What causes COPD?
In the United States, tobacco smoke is a key factor in the development and progression of COPD. Exposure to air pollutants in the home and workplace, genetic factors, and respiratory infections also play a role. In the developing world, indoor air quality is thought to play a larger role than it does in the United States. People should try to avoid inhaling tobacco smoke, home, and workplace air pollutants, and respiratory infections to prevent developing COPD. Early detection of COPD may change its course and progress.
Who is at risk?
Most people who are at risk for getting COPD have never even heard of it and, in many cases, don’t even realize that the condition has a name. Some of the things that put you at risk for COPD include:
Smoking
COPD most often occurs in people age 40 and over with a history of smoking (either current or former smokers), although as many as one out of four people with COPD never smoked. Smoking is the most common cause of COPD—it accounts for as many as eight out of ten COPD-related deaths.
Environmental Exposure
COPD can also occur in people who have had long-term exposure to things that can irritate your lungs, like certain chemicals, dust, or fumes in the workplace. Heavy or long-term exposure to secondhand smoke or other air pollutants may also contribute to COPD.
Genetic Factors
In some people, COPD is caused by a genetic condition known as alpha-1 antitrypsin, or AAT, deficiency. While very few people know they have AAT deficiency, it is estimated that close to 100,000 Americans have it. People with AAT deficiency can get COPD even if they have never smoked or had long-term exposure to harmful pollutants.
What are the complications or effects of COPD?
Compared to adults without COPD, those with this disease are more likely to:
-
- Have activity limitations like difficulty walking or climbing stairs.
- Be unable to work
- Need special equipment like portable oxygen tanks.
- Not engage in social activities like eating out, going to places of worship, going to group events, or getting together with friends or neighbors.
- Have increased confusion or memory loss.
- Have more emergency room visits or overnight hospital stays.
- Have other chronic diseases like arthritis, congestive heart failure, diabetes, coronary heart disease, stroke, or asthma.
- Have depression or other mental or emotional conditions.
- Report a fair or poor health status.
How is COPD diagnosed?
Spirometry
Spirometry is one of the best and most common lung function tests. The test is done with a spirometer, a machine that measures how well your lungs function, records the results and displays them on a graph. You will be asked to take a deep breath, then blow out as hard and as fast as you can using a mouthpiece connected to the machine with tubing. The spirometer then measures the total amount exhaled, called the forced vital capacity or FVC, and how much you exhaled in the first second, called the forced expiratory volume in 1 second or FEV1. Your doctor or healthcare provider will read the results to assess how well your lungs are working and whether or not you have COPD.
Spirometry can detect COPD before symptoms become severe. It is a simple, non-invasive breathing test that measures the amount of air a person can blow out of the lungs (volume) and how fast he or she can blow it out (flow). The test helps detect COPD and its severity and can also find out whether other conditions, such as asthma or heart failure, are causing the symptoms. Based on this test, your doctor or healthcare provider can tell if you have COPD, and if so, how severe it is. The spirometry reading can help them to determine the best course of treatment.
Other Tests
Your doctor may recommend other tests, such as:
-
- A chest x-ray or chest CT scan. These tests create pictures of the structures inside your chest, such as your heart, lungs, and blood vessels. The pictures can show signs of COPD. They also may show whether another condition, such as heart failure, is causing your symptoms.
- An arterial blood gas test. This blood test measures the oxygen level in your blood using a sample of blood taken from an artery. The results from this test can show how severe your COPD is and whether you need oxygen therapy.
How is COPD treated?
Treatment of COPD requires a careful and thorough evaluation by a physician.3,10 COPD treatment can alleviate symptoms, decrease the frequency and severity of exacerbations, and increase exercise tolerance. Treatment options that your physician may consider include:
-
- Quit smoking. For people who smoke, the most important part of treatment is smoking cessation.
- Avoid tobacco smoke and other air pollutants at home and at work.
- Ask your doctor about pulmonary rehabilitation, which is a personalized treatment program that teaches COPD management strategies to improve quality of life. Programs may include plans that teach people how to breathe better and conserve their energy, as well as provide advice on food and exercise.
- Take medication. Symptoms such as coughing or wheezing can be treated with medication.
- Avoid lung infections. Lung infections can cause serious problems in people with COPD. Certain vaccines, such as flu and pneumococcal vaccines, are especially important for people with COPD. Learn more about vaccination recommendations. Respiratory infections should be treated with antibiotics, if appropriate.
- Use supplemental oxygen. Some people may need to use a portable oxygen tank if their blood oxygen levels are low.
Source:
- National Heart, Lung and Blood Institute
- CDC
Picture:
- National Heart, Lung and Blood Institute
- CDC



Most Commented