
STD Risk and Oral Sex
Many sexually transmitted diseases (STDs) can be spread through oral sex. Using a condom, dental dam or other barrier method each and every time you have oral sex can reduce the risk of giving or getting an STD. Although oral sex may carry a lower risk for spreading HIV than other forms of sex, repeated unprotected exposures may increase risk of transmission.
What is Oral Sex?
Oral sex involves using the mouth, lips, or tongue to stimulate the penis (fellatio), vagina (cunnilingus), or anus (anilingus) of a sex partner. The penis and testicles and the vagina and area around the vagina are also called the genitals or genital area.
How Common is Oral Sex?
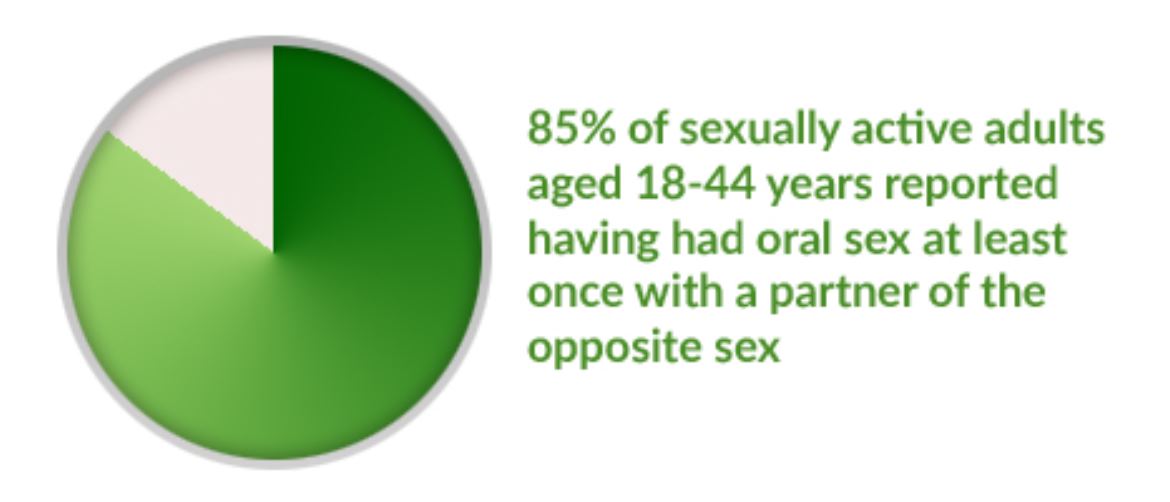
Oral sex is commonly practiced by sexually active adults. Oral sex can happen between heterosexual (straight) and same-sex (gay or lesbian) couples. More than 85% of sexually active adults aged 18-44 years reported having had oral sex at least once with a partner of the opposite sex.
Can STDs Be Spread During Oral Sex?
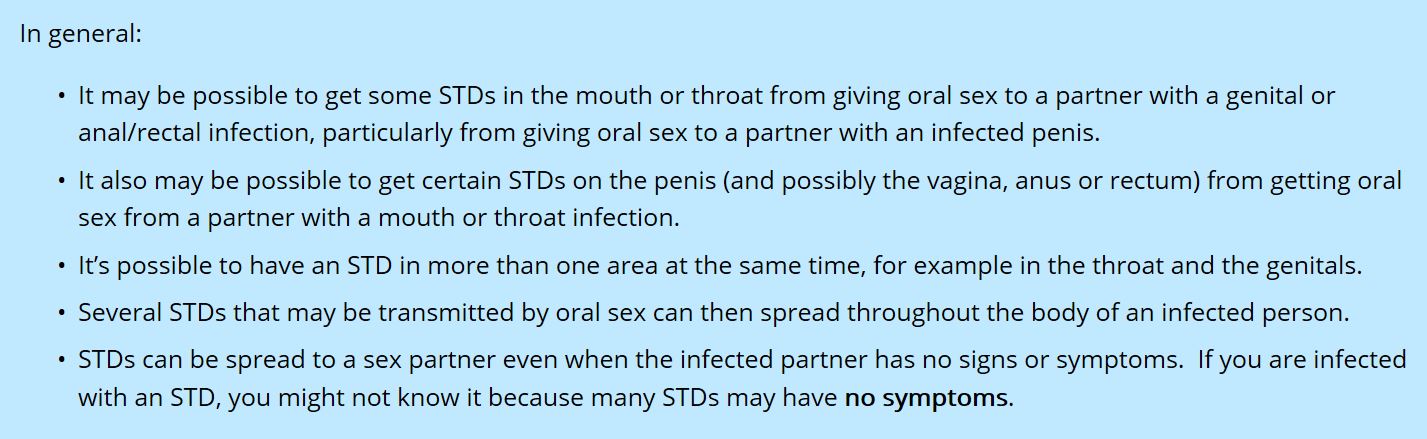
Many STDs, as well as other infections, can be spread through oral sex. Anyone exposed to an infected partner can get an STD in the mouth, throat, genitals, or rectum. The risk of getting an STD from oral sex, or spreading an STD to others through oral sex, depends on a number of things, including
- The particular STD.
- The sex acts practiced.
- How common the STD is in the population to which the sex partners belong.
- The number of specific sex acts performed.
Which STDs Can Be Passed On from Oral Sex?
[vc_tta_accordion color=”chino” active_section=”” collapsible_all=”true”]Risk of infection from oral sex:
- Giving oral sex to a man with an infected penis can result in getting chlamydia in the throat.
- Giving oral sex to a woman with an infected vagina or urinary tract may result in getting chlamydia in the throat.*
- Giving oral sex to a man or woman with an infected rectum might result in getting chlamydia in the throat.*
- Getting oral sex on the penis from a partner with chlamydia in the throat can result in getting chlamydia of the penis.
- Getting oral sex on the vagina from a partner with chlamydia in the throat might result in getting chlamydia of the vagina or urinary tract.*
- Getting oral sex on the anus from a partner with chlamydia in the throat might result in getting chlamydia in the rectum.*
* Statements followed by an asterisk (*) have not been well studied.
Areas of initial infection:
- Throat
- Genitals
- Urinary tract
- Rectum
Initial signs and symptoms of infection:
- Most chlamydia infections in the throat have no symptoms. When symptoms are present, they can include a sore throat.
- Many genital, urinary tract, or rectal chlamydia infections have no symptoms. When symptoms are present, they can include:
- Discharge from vagina or penis (discharge from the vagina may be bloody).
- Burning feeling when urinating.
- Painful or swollen testicles.
- Rectal pain or discharge
Treatment:
- Chlamydia can be cured with the right medicine.
- The sex partners of a person with chlamydia should also be tested for infection. Those who are diagnosed with chlamydia should not have sex until they and their sex partners have completed treatment.
If left untreated, throat infections:
- Can be spread to uninfected sex partners, particularly by performing oral sex on a male partner’s penis.
If left untreated, genital, urinary and/or rectal infections:
- Can be spread to uninfected sex partners.
In women:
- Can cause pelvic inflammatory disease (PID), which can lead to chronic pelvic pain, infertility, and ectopic pregnancy (a pregnancy in the fallopian tube or elsewhere outside of the womb).
In pregnant women:
- Might result in premature birth or low birth weight in babies.
- Can be spread to the baby during delivery, and can cause chlamydia infection in the eyes or infection of the respiratory tract that can develop into pneumonia.
In men:
- Can cause epididymitis, a painful condition of the ducts attached to the testicles that may lead to ductal scarring.
In both men and women:
- May increase risk of getting HIV infection.
- Might increase risk of spreading HIV to sex partners.
- May cause a reaction (reactive arthritis) throughout the body that can lead to arthritis (joint pain), conjunctivitis (pink eye), and/or a rash on the soles of the feet or elsewhere.
In addition to the STDs above, other infections such as hepatitis A virus, Shigella and intestinal parasites (amebiasis) can be spread through giving oral sex on the anus.
Risk of infection from oral sex:
- Giving oral sex to a man with an infected penis can result in getting gonorrhea in the throat.
- Giving oral sex to a woman with an infected vagina or urinary tract might result in getting gonorrhea in the throat.*
- Giving oral sex to a man or woman with an infected rectum might result in getting gonorrhea in the throat.*
- Getting oral sex on the penis from a partner with gonorrhea in the throat may result in getting gonorrhea of the penis.
- Getting oral sex on the vagina from a partner with gonorrhea in the throat might result in getting gonorrhea of the vagina or urinary tract.*
- Getting oral sex on the anus from a partner with gonorrhea in the throat might result in getting gonorrhea in the rectum.*
* Statements followed by an asterisk (*) have not been well studied.
Areas of initial infection:
- Throat
- Genitals
- Urinary tract
- Rectum
Initial signs and symptoms of infection:
- Most gonorrhea infections in the throat have no symptoms. When symptoms are present, they can include a sore throat.
- Symptoms of genital, urinary tract, or rectal infection may include:
- Discharge from vagina or penis (discharge from the vagina may be bloody).
- Burning feeling when urinating.
- Painful or swollen testicles.
- Rectal pain or discharge.
Treatment:
- Infections in the throat are harder to cure than genital or rectal infections but can be treated with recommended antibiotics.
- Genital and rectal infections can also be cured with the right medicine.
- The sex partners of a person with gonorrhea should also be tested for infection. Those who are diagnosed with gonorrhea should not have sex until they and their sex partners have completed treatment.
If left untreated, throat infections:
- Can be spread to uninfected sex partners.
- Might spread through the body causing skin sores and joint pain. This condition is called disseminated gonococcal infection. The heart can also be infected. This is a serious and potentially life-threatening condition.
If left untreated, genital, urinary and/or rectal infections:
- Can be spread to other sex partners.
In women:
- Can cause pelvic inflammatory disease (PID), which can lead to chronic pelvic pain, infertility, and ectopic pregnancy (a pregnancy in the fallopian tube or elsewhere outside of the womb).
In pregnant women:
- Can be spread to the baby during delivery, and can cause blindness, joint infection, or a life-threatening blood infection in the baby.
In men:
- Can cause epididymitis, a painful condition of the ducts attached to the testicles that may lead to ductal scarring.
In both men and women:
- May increase risk of getting HIV infection.
- Might increase risk of spreading HIV to sex partners.
- May spread through the body causing skin sores and joint pain. This condition is called disseminated gonococcal infection. The heart can also be infected, which is a serious and potentially life threatening condition.
In addition to the STDs above, other infections such as hepatitis A virus, Shigella and intestinal parasites (amebiasis) can be spread through giving oral sex on the anus.
Risk of infection from oral sex:
- Giving oral sex to a partner with a syphilis sore or rash on the genitals or anus can result in getting syphilis.
- Getting oral sex from a partner with a syphilis sore or rash on the lips or mouth, or in the throat, can result in getting syphilis.
- Another important factor that affects risk of spreading syphilis is how long an infected partner has had syphilis.
Areas of initial infection:
- Lips
- Mouth
- Throat
- Genitals
- Anus
- Rectum
Initial signs and symptoms of infection:
- May not have symptoms.
- One or more painless ulcers or sores on the lips, mouth, or throat; on the skin; or on or near the genitals or anus.
- Rash on trunk, palms of hands, and/or soles of feet.
- Flu-like symptoms.
Treatment:
- Syphilis can be cured with the right medicine.
- Sex partners of a person with syphilis should also be tested for infection, including some of the infected person’s past sex partners. Some of these partners should be treated even if their syphilis test results are negative.
If left untreated, syphilis:
- Can be spread to others through contact with syphilis sores or rash.
- In pregnant women:
- Can be spread to the baby during pregnancy.
- Can cause stillbirth (a baby born dead).
- Babies with untreated syphilis may become developmentally delayed, have seizures, or die.
- In both men and women:
- Can increase risk of getting HIV infection.
- Can increase risk of spreading HIV to sex partners.
- May cause damage to internal organs, blindness, muscle weakness, dementia, and even death.
In addition to the STDs above, other infections such as hepatitis A virus, Shigella and intestinal parasites (amebiasis) can be spread through giving oral sex on the anus.
Risk of infection from oral sex:
- Giving oral sex to a partner with herpes on the genital area, anus, buttocks, or in the rectum may result in getting herpes on the lips, mouth, or in the throat.
- Getting oral sex from a partner with herpes on the lips, mouth, or in the throat can result in getting herpes on the genital area, anus, buttocks, or in the rectum.
Areas of infection:
- Lips
- Mouth
- Throat
- Genital area
- Anus
- Rectum
- Buttocks
Signs and symptoms of infection:
- May not have symptoms.
- Headache or fever (during initial infection).
- Painful or itching sores at or near the area of infection.
Treatment:
- There is no cure for a herpes, but antiviral medicine can shorten and help decrease symptoms of herpes outbreaks.
- Daily antiviral medication can prevent or shorten herpes outbreaks.
Even with treatment, oral (lip, mouth and throat) infections:
- Can be spread to others, including sex partners.
Even with treatment, genital area, buttock, anal, and/or rectal infections:
- Can be spread to uninfected sex partners.
- In pregnant women:
- May be spread to the baby during delivery, and can cause brain damage, damage to internal organs, or even death of the baby.
- In both men and women:
- Can increase risk of getting HIV infection.
- Can increase risk of giving HIV to sex partners.
In addition to the STDs above, other infections such as hepatitis A virus, Shigella and intestinal parasites (amebiasis) can be spread through giving oral sex on the anus.
Risk of infection from oral sex:
- Giving oral sex to a man with an HPV-infected penis or genital area can result in getting HPV in the throat.
- Giving oral sex to a woman with an HPV-infected vagina or genital area can result in getting HPV in the throat.
- Giving oral sex to a man or woman with HPV on the anus or in the rectum may result in getting HPV in the throat.*
- Getting oral sex from a partner with HPV in the throat might result in getting HPV on the genital area, anus, or rectum.*
* Statements followed by an asterisk (*) have not been well studied.
Areas of infection:
- Mouth
- Throat
- Genital area
- Vagina
- Cervix
- Anus
- Rectum
Signs and symptoms of infection:
- May have no symptoms.
- Warts in the throat (laryngeal or respiratory papillomatosis):
- May cause changes in the voice, difficulty speaking, or shortness of breath.
- Genital or anal warts.
- Abnormal changes in cells of vagina, cervix, or anus that can be found by clinical examination and tests (Pap and/or HPV tests).
- Some types of HPV can lead to vaginal or cervical cancer, anal, penile, head, and neck cancers.
Vaccine:
- HPV vaccine protects against transmission of certain types of HPV.
- HPV vaccine is is recommended for 11- or 12-year-old girls, and for girls and women ages 13 through 26 years who have not yet been vaccinated with all recommended doses. Girls as young as age 9 years may be vaccinated.
- HPV vaccine is also recommended for 11- or 12-year-old boys, and for boys and men ages 13 through 21 years who have not yet been vaccinated with all recommended doses. Boys as young as age 9 years and men through age 26 years may also be vaccinated.
- Vaccination through age 26 years is recommended for men who have sex with men and for immunocompromised persons (including those who are living with HIV) who have not yet been vaccinated with all recommended doses.
Treatment:
- Warts in the mouth and throat:
- May disappear, remain unchanged, or grow in size or number.
- Surgery may be used to remove warts in the throat.
- Treatment may reduce warts but does not cure HPV infection.
- Genital and anal warts:
- May go away on their own, remain unchanged, or grow in size or number.
- Treatments include medicines applied to the warts, freezing the warts (cryotherapy), or surgery to remove the warts.
- Treatment may reduce warts but does not cure HPV infection.
- Abnormal changes in cells of vagina, cervix, or anus:
- May need more clinical examination and testing (Pap and/or HPV tests).
- Other procedures may be used, such as biopsy (taking a small sample of tissue) and/or removal of abnormal tissue, depending on age, pregnancy status, and test results.
Even with treatment, warts in the throat:
- Might be spread to uninfected sex partners.
- May have recurrences (recurrent respiratory papillomatosis).
Even with treatment, genital and anal warts:
- Can be spread to uninfected sex partners.
- May return but will not develop into cancer.
Mouth and throat infections by several types of HPV that do not cause warts may develop into head or neck cancer.
Abnormal changes in cells of vagina or anus:
- Might develop into cancer. Although some women have abnormal Pap and/or HPV test results, few women get cervical cancer if they get the appropriate follow-up and treatment.
In addition to the STDs above, other infections such as hepatitis A virus, Shigella and intestinal parasites (amebiasis) can be spread through giving oral sex on the anus.
Risk of infection from oral sex:
- Giving oral sex on the penis of a man with HIV can result in getting HIV. The risk of infection is lower than the risks from vaginal or anal sex.
- Giving oral sex on the vagina of a woman with HIV may result in getting HIV. The risk of infection is thought to be very low.
- Giving oral sex on the anus of a partner with HIV may result in getting HIV. There are few reports of transmission from this type of oral sex.
- Getting oral sex on the penis from a partner with HIV may result in getting HIV. This risk is thought to be very low, but has not been well studied.
- Getting oral sex on the vagina from a partner with HIV might result in getting HIV. This risk is thought to be extremely low, but has not been well studied.
- Getting oral sex on the anus from a partner with HIV might result in getting HIV. There are few reports of transmission from this type of oral sex.
- Another important factor that affects risk of HIV spread is the virus level (i.e., viral load) in an infected partner’s blood and other body fluids at the time of the sexual encounter. A low HIV viral load in an infected partner does not completely eliminate the risk of spreading HIV from oral sex.
Areas of infection:
- Iinfection of the immune system throughout the body.
Initial signs and symptoms of infection:
- May have no symptoms for many years.
- Flu-like symptoms.
Treatment
- There is no cure for HIV, but antiviral and other medicines can help people with HIV live longer with a better quality of life.
Even with treatment, HIV infection:
- Can be spread to uninfected sex partners.
- Can increase the risk of getting certain infections and cancers.
In addition to the STDs above, other infections such as hepatitis A virus, Shigella and intestinal parasites (amebiasis) can be spread through giving oral sex on the anus.
Risk of infection from oral sex:
- Giving oral sex to a woman with an infected vagina or a man with an infected penis might result in getting trichomoniasis of the throat. There are few reports of potential spread from oral sex.
- Spread of trichomoniasis by other oral sex practices has not been reported.
Areas of initial infection
- Vagina
- Penis
- Mouth/throat (possibly)
Initial signs and symptoms of infection
- Infections of the genitals or urinary tract may have no symptoms, especially in men
- Symptoms of genital or urinary tract infection can include:
- Discharge from vagina or penis.
- Vaginal area redness.
- Vaginal itching.
- Burning feeling when urinating.
Treatment
- Can be cured with right medicine.
- The sex partners of people with trichomoniasis should also be tested for infection. Those who are diagnosed with trichomoniasis should not have sex until they and their sex partners have completed treatment.
If left untreated, genital or urinary infections:
- Can be spread to uninfected sex partners.
In addition to the STDs above, other infections such as hepatitis A virus, Shigella and intestinal parasites (amebiasis) can be spread through giving oral sex on the anus.
Is Oral Sex Safer than Vaginal or Anal Sex?
- Many STDs can be spread through oral sex. However, it is difficult to compare the exact risks of getting specific STDs from specific types of sexual activity. This is partly because most people who have oral sex also have vaginal or anal sex. Also, few studies have looked at the risks of getting STDs other than HIV from giving oral sex on the vagina or anus, compared to giving oral sex on the penis.
- Studies have shown that the risk of getting HIV from having oral sex with an infected partner (either giving or getting oral sex) is much lower than the risk of getting HIV from anal or vaginal sex with an infected partner. This may not be true for other STDs – in one study of gay men with syphilis, 1 out of 5 reported having only oral sex.
- Getting HIV from oral sex may be less likely than vaginal or anal sex, but it still carries risk. If you are having oral sex you should still protect yourself. Repeated unprotected oral sex exposure to HIV may represent a considerable risk for spread of HIV, as well as other STDs for which the risk of spread through oral sex has not been as well studied.
- It is possible that getting certain STDs, such as chlamydia or gonorrhea, in the throat may not pose as great a threat to an infected person’s health as getting an STD in the genital area or rectum. Having these infections in the throat might increase the risk of getting HIV. Having gonorrhea in the throat also may lead to spread of the disease throughout the body. In addition:
- Having infections of chlamydia and gonorrhea in the throat may make it easier to spread these infections to others through oral sex. This is especially important for gonorrhea, since throat infections are harder to treat than urinary, genital or rectal infections.
- Infections from certain STDs, such as syphilis and HIV, spread throughout the body. Therefore, infections that are acquired in the throat may lead to the same health problems as infections acquired in the genitals or rectum.
- Mouth and throat infections by certain types of HPV may develop into oral or neck cancer.
What May Increase the Chances of Giving or Getting an STD through Oral Sex?
It is possible that certain factors may increase a person’s chances of getting HIV or other STDs during oral sex if exposed to an infected partner, such as:
- Having poor oral health which can include tooth decay, gum disease or bleeding gums, and oral cancer.
- Having sores in the mouth or on the genitals.
- Being exposed to the “pre-cum” or “cum” (also known as pre-ejaculate or ejaculate) of an infected partner.
However, no scientific studies have been done to show whether or not these factors actually do increase the risk of getting HIV or STDs from oral sex.
What Can You Do to Prevent STD Transmission During Oral Sex?
You can lower your chances of giving or getting STDs during oral sex by using a condom, dental dam or other barrier method each and every time you have oral sex.
- For oral sex on the penis:
- Cover the penis with a non-lubricated latex condom.
- Use plastic (polyurethane) condoms if you or your partner is allergic to latex.
- For oral sex on the vagina or anus:
- Use a dental dam.
- Cut open a condom to make a square, and put it between the mouth and the partner’s vagina or anus.
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting an STD:
- Being in a long-term mutually monogamous relationship with a partner who is not infected with an STD (e.g., a partner who has been tested and has negative STD test results).
- Using latex condoms the right way every time you have sex.
It’s important to remember that many infected individuals may be unaware of their infection because STDs often have no symptoms and are unrecognized.
Source:
- CDC
Images:
- CDC


Most Commented